26 Chapter 26: Hormones, Growth, and Development
Anastasia Chouvalova
Learning Objectives
By the end of this section, students should be able to:
26.1 Compare and contrast peptide/protein hormones with steroidal hormones.
26.2 Be able to explain how plants respond to their environment given their immobility and the role of hormones in these processes.
26.3 Construct a model that demonstrates your understanding of calcium and glucose homeostasis in humans.
26.4 Be able to predict outcomes associated with deficiencies in hormones in plants and animals (i.e., auxin, growth hormone).
Introduction to the Endocrine System
An animal’s endocrine system controls body processes through the production, secretion, and regulation of hormones, which serve as chemical “messengers” functioning in cellular and organ activity and, ultimately, maintaining the body’s homeostasis. The endocrine system plays a role in growth, metabolism, and sexual development. In humans, common endocrine system diseases include thyroid disease and diabetes mellitus. In organisms that undergo metamorphosis, the process is controlled by the endocrine system. The transformation from tadpole to frog, for example, is complex and nuanced to adapt to specific environments and ecological circumstances.

Different Types of Hormones
Maintaining homeostasis within the body requires the coordination of many different systems and organs. Communication between neighboring cells, and between cells and tissues in distant parts of the body, occurs through the release of chemicals called hormones. Hormones are released into body fluids (usually blood) that carry these chemicals to their target cells. At the target cells, which are cells that have a receptor for a signal or ligand from a signal cell, the hormones elicit a response. The cells, tissues, and organs that secrete hormones make up the endocrine system. Examples of glands of the endocrine system include the adrenal glands, which produce hormones such as epinephrine and norepinephrine that regulate responses to stress, and the thyroid gland, which produces thyroid hormones that regulate metabolic rates.
Although there are many different hormones in the human body, they can be divided into three classes based on their chemical structure: lipid-derived, amino acid-derived, and peptide (peptide and proteins) hormones. One of the key distinguishing features of lipid-derived hormones is that they can diffuse across plasma membranes whereas the amino acid-derived and peptide hormones cannot.
Lipid-Derived Hormones (or Lipid-soluble Hormones)
Most lipid hormones are derived from cholesterol and thus are structurally similar to it, as illustrated in Figure 21.2. The primary class of lipid hormones in humans is the steroid hormones. Chemically, these hormones are usually ketones or alcohols; their chemical names will end in “-ol” for alcohols or “-one” for ketones. Examples of steroid hormones include estrogens (such as estradiol) and androgens (such as testosterone), both of which regulate bone and tissue development in all humans.
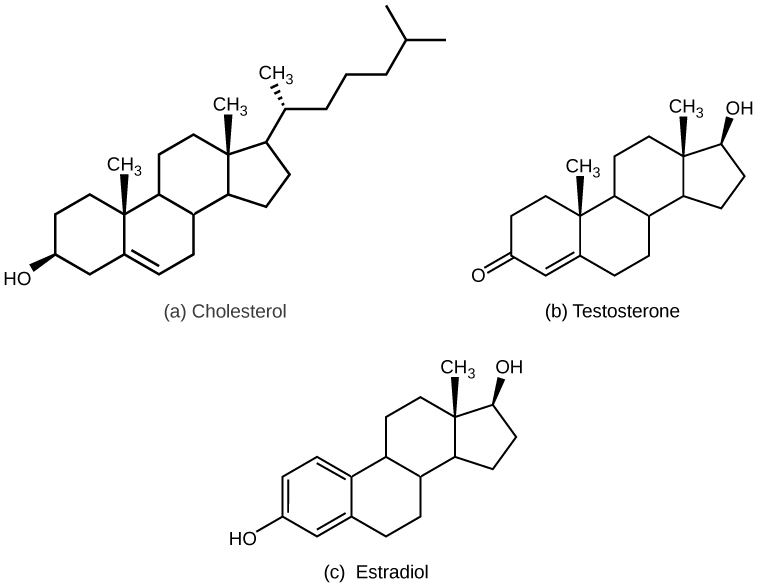
Gonadal hormones, produced by the gonads, include both steroid and peptide hormones. Androgens and estrogens resemble one another in chemical structure and originate from the same molecule. Estrogens are chief drivers of sexual development in an ovarian reproductive system, while androgens drive development in a testicular reproductive system. The ovaries produce steroid hormones such as estradiol and progesterone. When androgens are produced, some of them are later converted to estrogens. Minute amounts of estrogen occur through aromatase actions in adipose, brain, skin, and bone, which convert testosterone to estrogen. The testes and the adrenal cortex both secrete testosterone.
Other steroid hormones include aldosterone and cortisol, which are released by the adrenal glands along with some other types of androgens. Steroid hormones are insoluble in water, and they are transported by transport proteins in blood. As a result, they remain in circulation longer than peptide hormones. For example, cortisol has a half-life of 60 to 90 minutes, while epinephrine, an amino acid derived-hormone, has a half-life of approximately one minute.
Reading Question #1
Which of the following is not a class of hormone?
A. Peptide
B. Amino-acid derived
C. Lipid-soluble hormone
D. Cortisol
Amino Acid-Derived Hormones
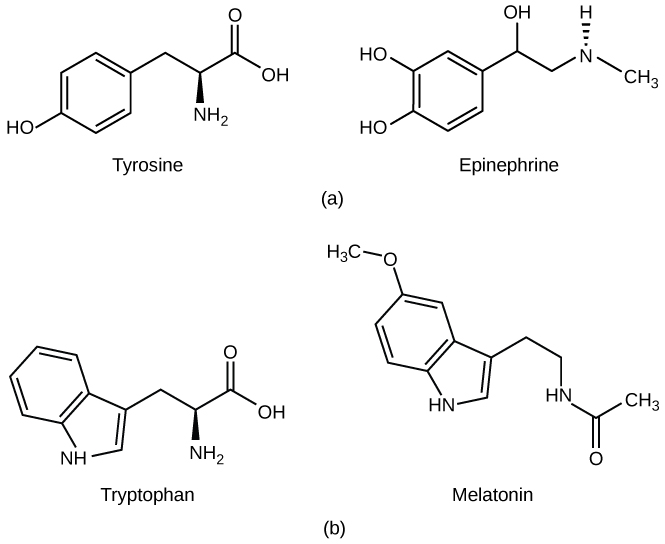
The amino acid-derived hormones are relatively small molecules that are derived from the amino acids tyrosine and tryptophan, shown in Figure 21.3. If a hormone is amino acid-derived, its chemical name will end in “-ine”. Examples of amino acid-derived hormones include epinephrine and norepinephrine, which are synthesized in the medulla of the adrenal glands, and thyroxine, which is produced by the thyroid gland. The pineal gland in the brain makes and secretes melatonin which regulates sleep cycles.
Peptide Hormones
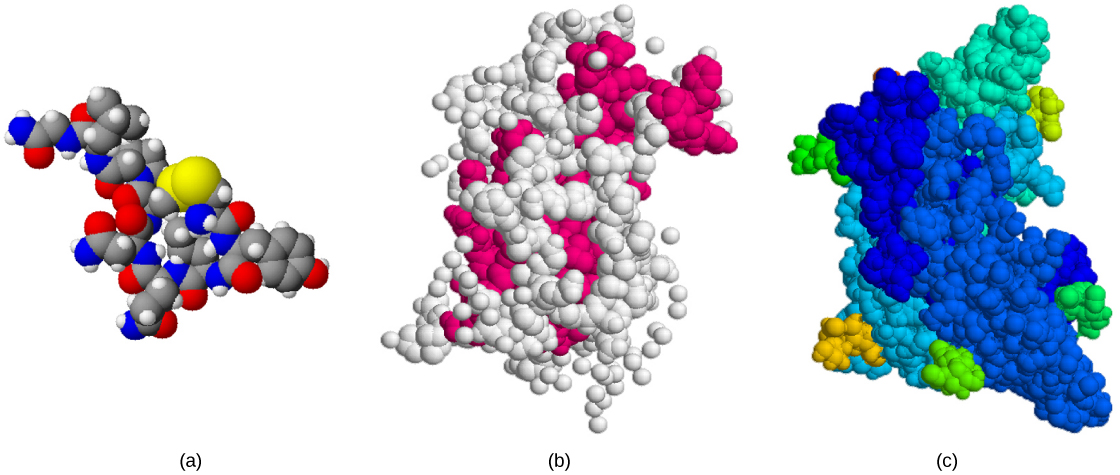
The structure of peptide hormones is that of a polypeptide chain (chain of amino acids). The peptide hormones include molecules that are short polypeptide chains, such as antidiuretic hormone and oxytocin produced in the brain and released into the blood in the posterior pituitary gland. This class also includes small proteins, like growth hormones produced by the pituitary, and large glycoproteins such as follicle-stimulating hormone produced by the pituitary. Figure 21.4 illustrates these peptide hormones.
Reading Question #2
Researchers at Texas Tech University Health Sciences Centre may have discovered a novel hormone that they have called Hormone X. Here are some of its properties:
- It is a steroid hormone that resembles testosterone.
- This hormone is produced by the testes.
- When detected in the bloodstream, it is attached to transport proteins.
- It has a long half-life.
Based on this description, which of the following is Hormone X most likely to be an example of? Choose all that apply.
A. Lipid-soluble hormone
B. Peptide
C. Amino-acid derived
D. Gonadal
Career Connection
Endocrinologist
An endocrinologist is a medical doctor who specializes in treating disorders of the endocrine glands, hormone systems, and glucose and lipid metabolic pathways. An endocrine surgeon specializes in the surgical treatment of endocrine diseases and glands. Some of the diseases that are managed by endocrinologists: disorders of the pancreas (diabetes mellitus), disorders of the pituitary (gigantism, acromegaly, and pituitary dwarfism), disorders of the thyroid gland (goiter and Graves’ disease), and disorders of the adrenal glands (Cushing’s disease and Addison’s disease).
Endocrinologists are required to assess patients and diagnose endocrine disorders through extensive use of laboratory tests. Many endocrine diseases are diagnosed using tests that stimulate or suppress endocrine organ functioning. Blood samples are then drawn to determine the effect of stimulating or suppressing an endocrine organ on the production of hormones. For example, to diagnose diabetes mellitus, patients are required to fast for 12 to 24 hours. They are then given a sugary drink, which stimulates the pancreas to produce insulin to decrease blood glucose levels. A blood sample is taken one to two hours after the sugar drink is consumed. If the pancreas is functioning properly, the blood glucose level will be within a normal range. Another example is the A1C test, which can be performed during blood screening. The A1C test measures average blood glucose levels over the past two to three months by examining how well the blood glucose is being managed over a long time.
Once a disease has been diagnosed, endocrinologists can prescribe lifestyle changes and/or medications to treat the disease. Some cases of diabetes mellitus can be managed by exercise, weight loss, and a healthy diet; in other cases, medications may be required to enhance insulin release. If the disease cannot be controlled by these means, the endocrinologist may prescribe insulin injections.
In addition to clinical practice, endocrinologists may also be involved in primary research and development activities. For example, ongoing islet transplant research is investigating how healthy pancreas islet cells may be transplanted into diabetic patients. Successful islet transplants may allow patients to stop taking insulin injections.
How hormones work
Hormones mediate changes in target cells by binding to specific hormone receptors. In this way, even though hormones circulate throughout the body and come into contact with many different cell types, they only affect cells that possess the necessary receptors. Receptors for a specific hormone may be found on many different cells or may be limited to a small number of specialized cells. For example, thyroid hormones act on many different tissue types, stimulating metabolic activity throughout the body. Cells can have many receptors for the same hormone but often also possess receptors for different types of hormones. The number of receptors that respond to a hormone determines the cell’s sensitivity to that hormone, and the resulting cellular response. Additionally, the number of receptors that respond to a hormone can change over time, resulting in increased or decreased cell sensitivity. In up-regulation, the number of receptors increases in response to rising hormone levels, making the cell more sensitive to the hormone and allowing for more cellular activity. When the number of receptors decreases in response to rising hormone levels, called down-regulation, cellular activity is reduced.
Receptor binding alters cellular activity and results in an increase or decrease in normal body processes. Depending on the location of the protein receptor on the target cell and the chemical structure of the hormone, hormones can mediate changes directly by binding to intracellular hormone receptors and modulating gene transcription, or indirectly by binding to cell surface receptors and stimulating signaling pathways.
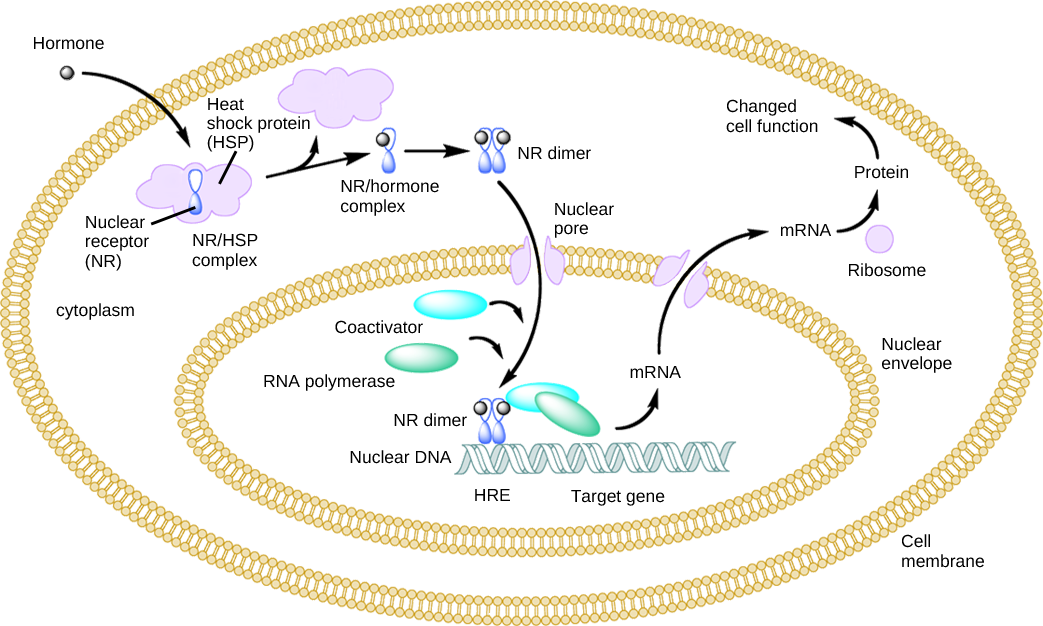
Intracellular Hormone Receptors
Lipid-derived (soluble) hormones such as steroid hormones diffuse across the membranes of the endocrine cell. Once outside the cell, they bind to transport proteins that keep them soluble in the bloodstream. At the target cell, the hormones are released from the carrier protein and diffuse across the lipid bilayer of the plasma membrane of cells. The steroid hormones pass through the plasma membrane of a target cell and adhere to intracellular receptors residing in the cytoplasm or in the nucleus. The cell signaling pathways induced by the steroid hormones regulate specific genes on the cell’s DNA. The hormones and receptor complex act as transcription regulators by increasing or decreasing the synthesis of mRNA molecules of specific genes. This, in turn, determines the amount of corresponding protein that is synthesized by altering gene expression. This protein can be used either to change the structure of the cell or to produce enzymes that catalyze chemical reactions. In this way, the steroid hormone regulates specific cell processes as illustrated in Figure 21.5.
Plasma Membrane Hormone Receptors
Amino acid-derived hormones (with the exception of thyroxine) and polypeptide hormones are not lipid-derived (lipid-soluble) and therefore cannot diffuse through the plasma membrane of cells. Lipid insoluble hormones bind to receptors on the outer surface of the plasma membrane, via plasma membrane hormone receptors. Unlike steroid hormones, lipid insoluble hormones do not directly affect the target cell because they cannot enter the cell and act directly on DNA. Binding of these hormones to a cell surface receptor results in activation of a signaling pathway; this triggers intracellular activity and carries out the specific effects associated with the hormone. In this way, nothing passes through the cell membrane; the hormone that binds at the surface remains at the surface of the cell while the intracellular product remains inside the cell.
Reading Question #3
Which type of hormone is epinephrine; which hormone receptor does it bind to?
A. Lipid-soluble hormone; plasma membrane hormone receptor
B. Peptide derived hormone; plasma membrane hormone receptor
C. Amino acid derived hormone; plasma membrane hormone receptor
D. Lipid-soluble hormone; intracellular hormone receptor
E. Peptide derived hormone; intracellular hormone receptor
F. Amino acid derived hormone; intracellular hormone receptor
Role of hormones in physiological processes
Hormones have a wide range of effects and modulate many different body processes. The key regulatory processes that will be examined here are those affecting the growth process and the stress response.
Hormonal Regulation of Growth
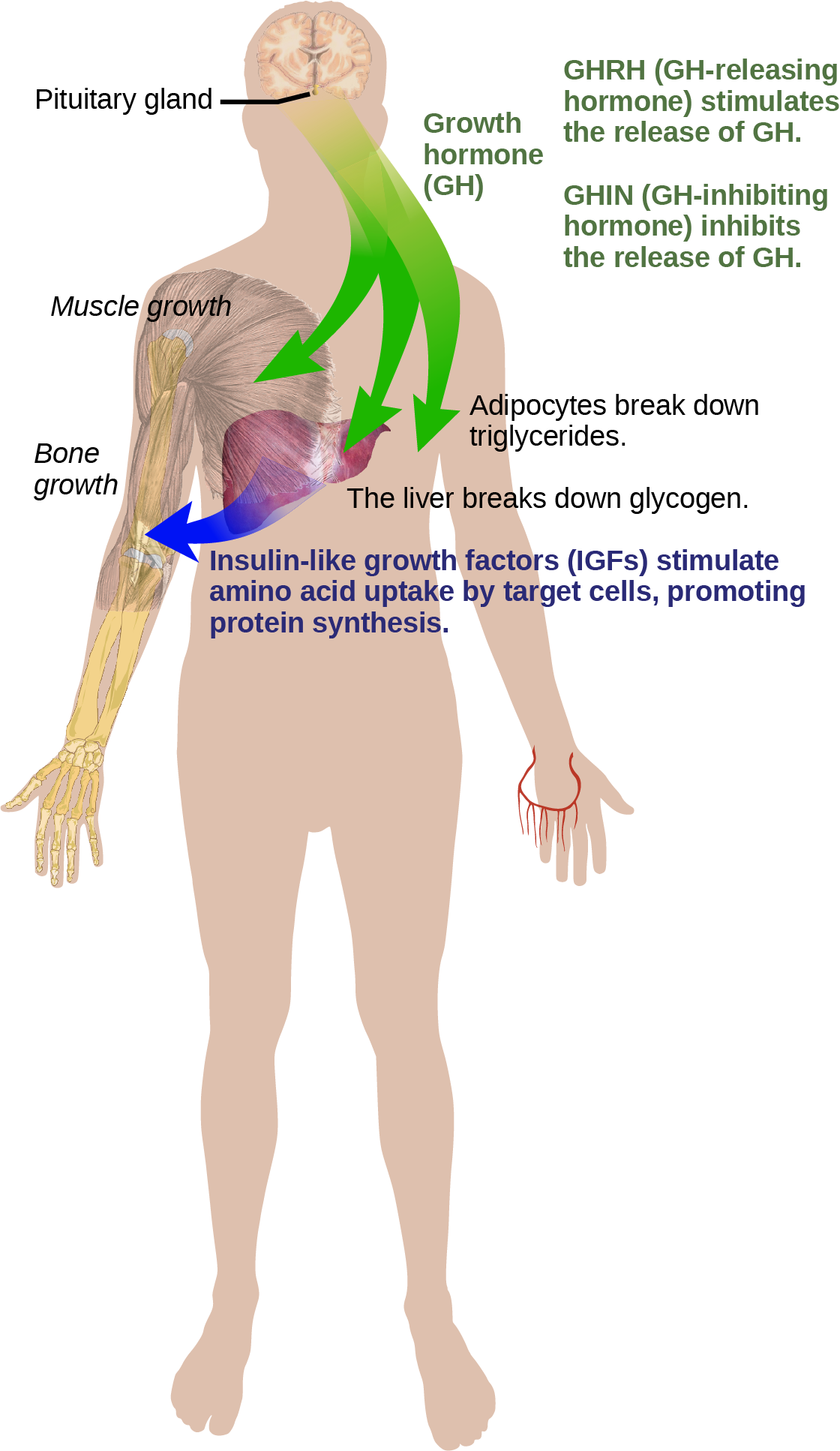
Hormonal regulation is required for the growth and replication of most cells in the body. Growth hormone (GH), produced by the anterior portion of the pituitary gland, accelerates the rate of protein synthesis, particularly in skeletal muscle and bones. Growth hormone has direct and indirect mechanisms of action. The first direct action of GH is stimulation of triglyceride breakdown (lipolysis) and release into the blood by adipocytes. This results in a switch by most tissues from utilizing glucose as an energy source to utilizing fatty acids. This process is called a glucose-sparing effect. In another direct mechanism, GH stimulates glycogen breakdown in the liver; the glycogen is then released into the blood as glucose. Blood glucose levels increase as most tissues are utilizing fatty acids instead of glucose for their energy needs. The GH mediated increase in blood glucose levels is called a diabetogenic effectbecause it is similar to the high blood glucose levels seen in diabetes mellitus.
The indirect mechanism of GH action is mediated by insulin-like growth factors (IGFs) or somatomedins, which are a family of growth-promoting proteins produced by the liver, which stimulates tissue growth. IGFs stimulate the uptake of amino acids from the blood, allowing the formation of new proteins, particularly in skeletal muscle cells, cartilage cells, and other target cells, as shown in Figure 21.6. This is especially important after a meal, when glucose and amino acid concentration levels are high in the blood. GH levels are regulated by two hormones produced by the hypothalamus. GH release is stimulated by growth hormone-releasing hormone (GHRH) and is inhibited by growth hormone-inhibiting hormone (GHIH), also called somatostatin.
A balanced production of growth hormone is critical for proper development. Underproduction of GH in adults does not appear to cause any abnormalities, but in children it can result in pituitary dwarfism, in which growth is reduced. Pituitary dwarfism is characterized by symmetric body formation. In some cases, individuals are under 30 inches in height. Oversecretion of growth hormone can lead to gigantism in children, causing excessive growth. In some documented cases, individuals can reach heights of over eight feet. In adults, excessive GH can lead to acromegaly, a condition in which there is enlargement of bones in the face, hands, and feet that are still capable of growth.
Hormonal Regulation of Stress
When a threat or danger is perceived, the body responds by releasing hormones that will ready it for the “fight-or-flight” response. The effects of this response are familiar to anyone who has been in a stressful situation: increased heart rate, dry mouth, and hair standing up.
Evolution Connection
Fight-or-Flight Response
Interactions of the endocrine hormones have evolved to ensure the body’s internal environment remains stable. Stressors are stimuli that disrupt homeostasis. The sympathetic division of the vertebrate autonomic nervous system has evolved the fight-or-flight response to counter stress-induced disruptions of homeostasis. In the initial alarm phase, the sympathetic nervous system stimulates an increase in energy levels through increased blood glucose levels. This prepares the body for physical activity that may be required to respond to stress: to either fight for survival or to flee from danger.
However, some stresses, such as illness or injury, can last for a long time. Glycogen reserves, which provide energy in the short-term response to stress, are exhausted after several hours and cannot meet long-term energy needs. If glycogen reserves were the only energy source available, neural functioning could not be maintained once the reserves became depleted due to the nervous system’s high requirement for glucose. In this situation, the body has evolved a response to counter long-term stress through the actions of the glucocorticoids, which ensure that long-term energy requirements can be met. The glucocorticoids mobilize lipid and protein reserves, stimulate gluconeogenesis, conserve glucose for use by neural tissue, and stimulate the conservation of salts and water. The mechanisms to maintain homeostasis that are described here are those observed in the human body. However, the fight-or-flight response exists in some form in all vertebrates.
The sympathetic nervous system regulates the stress response via the hypothalamus. Stressful stimuli cause the hypothalamus to signal the adrenal medulla (which mediates short-term stress responses) via nerve impulses, and the adrenal cortex, which mediates long-term stress responses, via the hormone adrenocorticotropic hormone (ACTH), which is produced by the anterior pituitary.
Short-term Stress Response
When presented with a stressful situation, the body responds by calling for the release of hormones that provide a burst of energy. The hormones epinephrine (also known as adrenaline) and norepinephrine (also known as noradrenaline) are released by the adrenal medulla. How do these hormones provide a burst of energy? Epinephrine and norepinephrine increase blood glucose levels by stimulating the liver and skeletal muscles to break down glycogen and by stimulating glucose release by liver cells. Additionally, these hormones increase oxygen availability to cells by increasing the heart rate and dilating the bronchioles. The hormones also prioritize body function by increasing blood supply to essential organs such as the heart, brain, and skeletal muscles, while restricting blood flow to organs not in immediate need, such as the skin, digestive system, and kidneys. Epinephrine and norepinephrine are collectively called catecholamines.
Long-term Stress Response
Long-term stress response differs from short-term stress response. The body cannot sustain the bursts of energy mediated by epinephrine and norepinephrine for long times. Instead, other hormones come into play. In a long-term stress response, the hypothalamus triggers the release of ACTH from the anterior pituitary gland. The adrenal cortex is stimulated by ACTH to release steroid hormones called corticosteroids. Corticosteroids turn on transcription of certain genes in the nuclei of target cells. They change enzyme concentrations in the cytoplasm and affect cellular metabolism. There are two main corticosteroids: glucocorticoids such as cortisol, and mineralocorticoids such as aldosterone. These hormones target the breakdown of fat into fatty acids in the adipose tissue. The fatty acids are released into the bloodstream for other tissues to use for ATP production. The glucocorticoids primarily affect glucose metabolism by stimulating glucose synthesis. Glucocorticoids also have anti-inflammatory properties through inhibition of the immune system. For example, cortisone is used as an anti-inflammatory medication; however, it cannot be used long term as it increases susceptibility to disease due to its immune-suppressing effects.
Mineralocorticoids function to regulate ion and water balance of the body. The hormone aldosterone stimulates the reabsorption of water and sodium ions in the kidney, which results in increased blood pressure and volume.
Hypersecretion of glucocorticoids can cause a condition known as Cushing’s disease, characterized by a shifting of fat storage areas of the body. This can cause the accumulation of adipose tissue in the face and neck, and excessive glucose in the blood. Hyposecretion of the corticosteroids can cause Addison’s disease, which may result in bronzing of the skin, hypoglycemia, and low electrolyte levels in the blood.
Regulation of Hormone Production
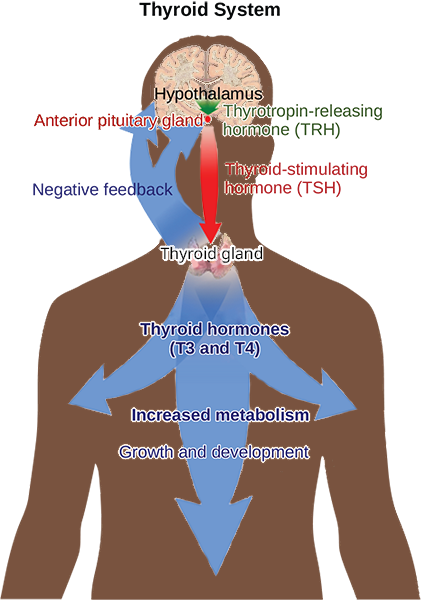
Hormone production and release are primarily controlled by negative feedback. In negative feedback systems, a stimulus elicits the release of a substance; once the substance reaches a certain level, it sends a signal that stops further release of the substance. In this way, the concentration of hormones in blood is maintained within a narrow range. For example, the anterior pituitary signals the thyroid to release thyroid hormones. Increasing levels of these hormones in the blood then give feedback to the hypothalamus and anterior pituitary to inhibit further signaling to the thyroid gland, as illustrated in Figure 21.7. There are three mechanisms by which endocrine glands are stimulated to synthesize and release hormones: humoral stimuli, hormonal stimuli, and neural stimuli.
Humoral Stimuli
The term “humoral” is derived from the term “humor,” which refers to bodily fluids such as blood. A humoral stimulus refers to the control of hormone release in response to changes in extracellular fluids such as blood or the ion concentration in the blood. For example, a rise in blood glucose levels triggers the pancreatic release of insulin. Insulin causes blood glucose levels to drop, which signals the pancreas to stop producing insulin in a negative feedback loop.
Hormonal Stimuli
Hormonal stimuli refers to the release of a hormone in response to another hormone. A number of endocrineglands release hormones when stimulated by hormones released by other endocrine glands. For example, the hypothalamus produces hormones that stimulate the anterior portion of the pituitary gland. The anterior pituitary in turn releases hormones that regulate hormone production by other endocrine glands. The anterior pituitary releases the thyroid-stimulating hormone, which then stimulates the thyroid gland to produce the hormones T3 and T4. As blood concentrations of T3 and T4 rise, they inhibit both the pituitary and the hypothalamus in a negative feedback loop.
Neural Stimuli
In some cases, the nervous system directly stimulates endocrine glands to release hormones, which is referred to as neural stimuli. Recall that in a short-term stress response, the hormones epinephrine and norepinephrine are important for providing the bursts of energy required for the body to respond. Here, neuronal signaling from the sympathetic nervous system directly stimulates the adrenal medulla to release the hormones epinephrine and norepinephrine in response to stress.
Reading Question #4
Which hormone is primarily responsible for calcium homeostasis when blood calcium levels are too high?
A. Glucagon
B. Insulin
C. Calcitonin
D. Parathyroid hormone
Endocrine Glands
Both the endocrine and nervous systems use chemical signals to communicate and regulate the body’s physiology. The endocrine system releases hormones that act on target cells to regulate development, growth, energy metabolism, reproduction, and many behaviors. The nervous system releases neurotransmitters or neurohormones that regulate neurons, muscle cells, and endocrine cells. Because the neurons can regulate the release of hormones, the nervous and endocrine systems work in a coordinated manner to regulate the body’s physiology.
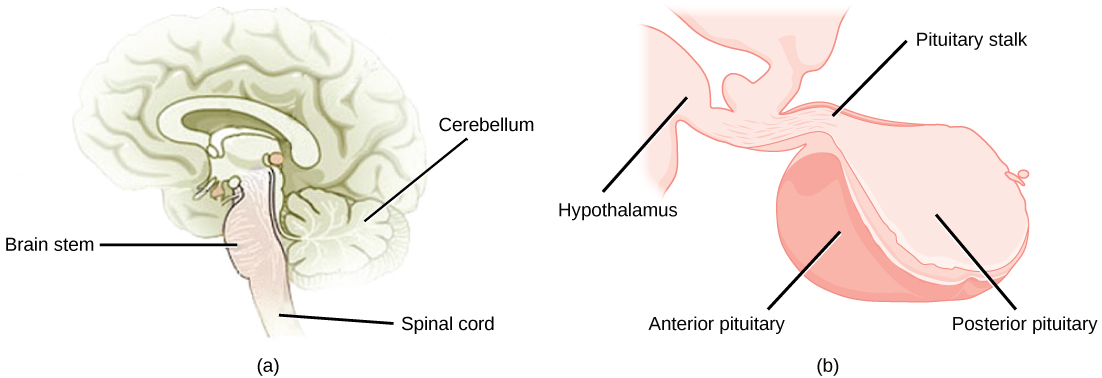
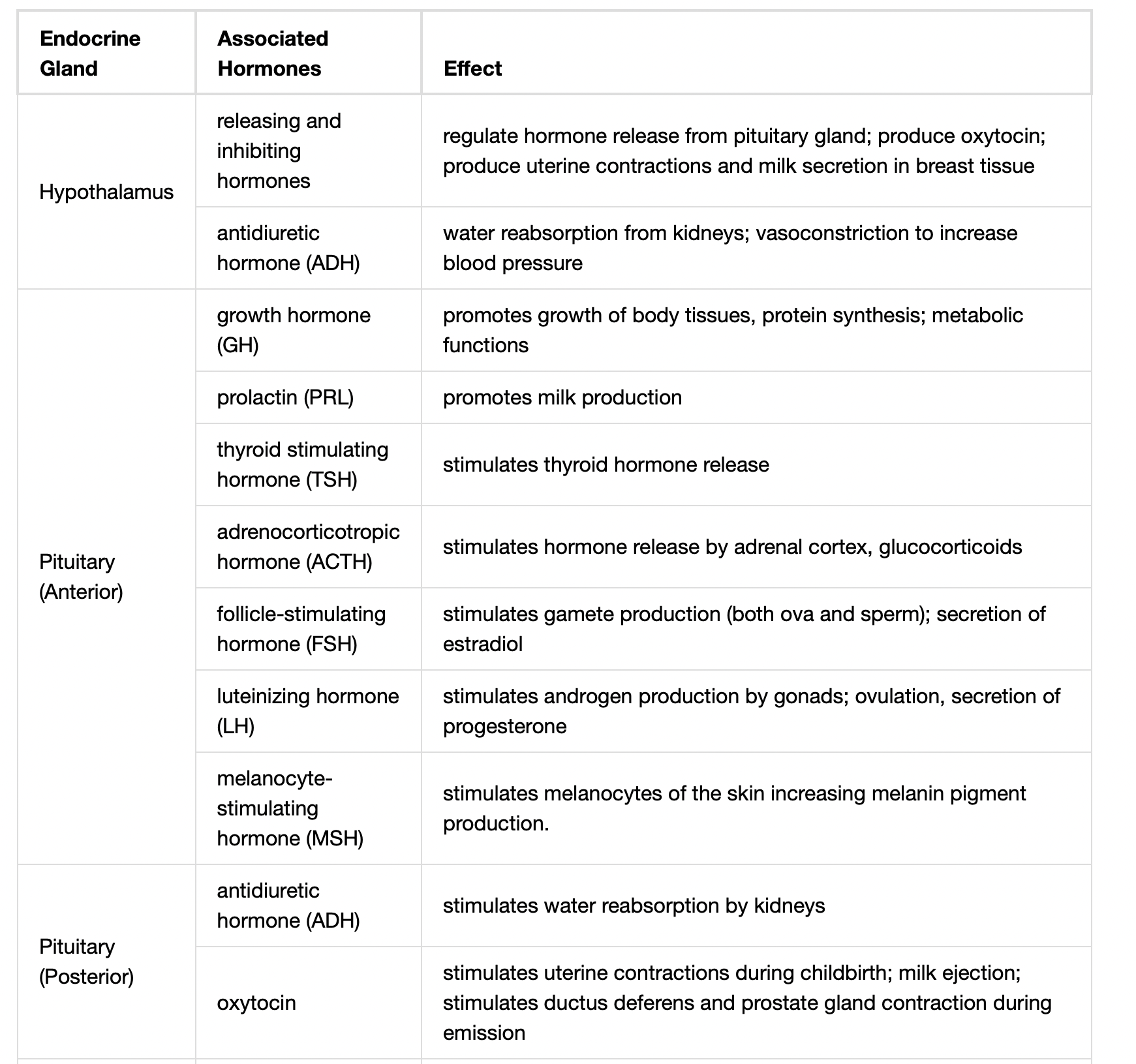
Hypothalamic-Pituitary Axis
The hypothalamus in vertebrates integrates the endocrine and nervous systems. The hypothalamus is an endocrine organ located in the diencephalon of the brain. It receives input from the body and other brain areas and initiates endocrine responses to environmental changes. The hypothalamus acts as an endocrine organ, synthesizing hormones and transporting them along axons to the posterior pituitary gland. It synthesizes and secretes regulatory hormones that control the endocrine cells in the anterior pituitary gland. The hypothalamus contains autonomic centers that control endocrine cells in the adrenal medulla via neuronal control.
The pituitary gland, sometimes called the hypophysis or “master gland” is located at the base of the brain in the sella turcica, a groove of the sphenoid bone of the skull, illustrated in Figure 21.8. It is attached to the hypothalamus via a stalk called the pituitary stalk (or infundibulum). The anterior portion of the pituitary gland is regulated by releasing or release-inhibiting hormones produced by the hypothalamus, and the posterior pituitary receives signals via neurosecretory cells to release hormones produced by the hypothalamus. The pituitary has two distinct regions—the anterior pituitary and the posterior pituitary—which between them secrete nine different peptide or protein hormones. The posterior lobe of the pituitary gland contains axons of the hypothalamic neurons.
Anterior Pituitary
The anterior pituitary gland, or adenohypophysis, is surrounded by a capillary network that extends from the hypothalamus, down along the infundibulum, and to the anterior pituitary. This capillary network is a part of the hypophyseal portal system that carries substances from the hypothalamus to the anterior pituitary and hormones from the anterior pituitary into the circulatory system. A portal system carries blood from one capillary network to another; therefore, the hypophyseal portal system allows hormones produced by the hypothalamus to be carried directly to the anterior pituitary without first entering the circulatory system.
The anterior pituitary produces seven hormones: growth hormone (GH), prolactin (PRL), thyroid-stimulating hormone (TSH), melanin-stimulating hormone (MSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH). Anterior pituitary hormones are sometimes referred to as tropic hormones, because they control the functioning of other organs. While these hormones are produced by the anterior pituitary, their production is controlled by regulatory hormones produced by the hypothalamus. These regulatory hormones can be releasing hormones or inhibiting hormones, causing more or less of the anterior pituitary hormones to be secreted. These travel from the hypothalamus through the hypophyseal portal system to the anterior pituitary where they exert their effect. Negative feedback then regulates how much of these regulatory hormones are released and how much anterior pituitary hormone is secreted.
Posterior Pituitary
The posterior pituitary is significantly different in structure from the anterior pituitary. It is a part of the brain, extending down from the hypothalamus, and contains mostly nerve fibers and neuroglial cells, which support axons that extend from the hypothalamus to the posterior pituitary. The posterior pituitary and the infundibulum together are referred to as the neurohypophysis.
The hormones antidiuretic hormone (ADH), also known as vasopressin, and oxytocin are produced by neurons in the hypothalamus and transported within these axons along the infundibulum to the posterior pituitary. They are released into the circulatory system via neural signaling from the hypothalamus. These hormones are considered to be posterior pituitary hormones, even though they are produced by the hypothalamus, because that is where they are released into the circulatory system. The posterior pituitary itself does not produce hormones, but instead stores hormones produced by the hypothalamus and releases them into the bloodstream.
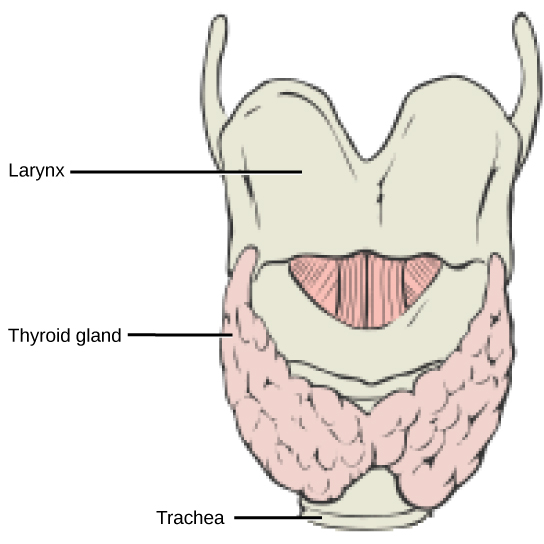
Thyroid Gland
The thyroid gland is located in the neck, just below the larynx and in front of the trachea, as shown in Figure 21.9. It is a butterfly-shaped gland with two lobes that are connected by the isthmus. It has a dark red color due to its extensive vascular system. When the thyroid swells due to dysfunction, it can be felt under the skin of the neck.
Thyroid follicle cells synthesize the hormone thyroxine, which is also known as T4 because it contains four atoms of iodine, and triiodothyronine, also known as T3 because it contains three atoms of iodine. Follicle cells are stimulated to release stored T3 and T4 by thyroid stimulating hormone (TSH), which is produced by the anterior pituitary. These thyroid hormones increase the rates of mitochondrial ATP production.
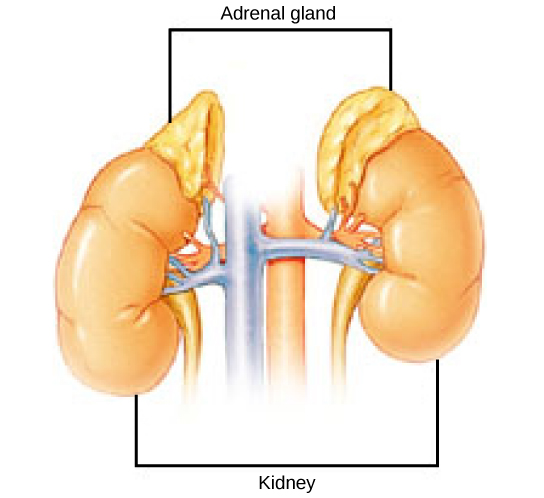
Adrenal Glands
The adrenal glands are associated with the kidneys; one gland is located on top of each kidney as illustrated in Figure 21.10. The adrenal glands consist of an outer adrenal cortex and an inner adrenal medulla. These regions secrete different hormones.
Adrenal Cortex
The adrenal cortex is made up of layers of epithelial cells and associated capillary networks. These layers form three distinct regions: an outer zona glomerulosa that produces mineralocorticoids, a middle zona fasciculata that produces glucocorticoids, and an inner zona reticularis that produces androgens.
The main mineralocorticoid is aldosterone, which regulates the concentration of Na+ ions in urine, sweat, pancreas, and saliva. Aldosterone release from the adrenal cortex is stimulated by a decrease in blood concentrations of sodium ions, blood volume, or blood pressure, or by an increase in blood potassium levels.
The three main glucocorticoids are cortisol, corticosterone, and cortisone. The glucocorticoids stimulate the synthesis of glucose and gluconeogenesis (converting a non-carbohydrate to glucose) by liver cells and they promote the release of fatty acids from adipose tissue. These hormones increase blood glucose levels to maintain levels within a normal range between meals. These hormones are secreted in response to ACTH and levels are regulated by negative feedback.
The adrenal cortex also produces small amounts of testosterone precursor, although the role of this additional hormone production is not fully understood. Testosterone is a type of androgen that is mainly produced by the gonads in both males and females, and promotes a suite of characteristics such as the growth and development of the testes and penis, increased skeletal and muscular growth, enlargement of the larynx, increased growth and redistribution of body hair, and increased sexual drive. Testosterone secretion is regulated by both the hypothalamus and the anterior pituitary gland. The hypothalamus sends releasing hormones that stimulate the release of gonadotropins from the anterior pituitary gland. Testosterone produced in small amounts in the adrenal cortex may work with sex hormones released from the gonads.
Adrenal Medulla
The adrenal medulla contains large, irregularly shaped cells that are closely associated with blood vessels. These cells are innervated by preganglionic autonomic nerve fibers from the central nervous system.
The adrenal medulla contains two types of secretory cells: one that produces epinephrine (adrenaline) and another that produces norepinephrine (noradrenaline). Epinephrine is the primary adrenal medulla hormone accounting for 75 to 80 percent of its secretions. Epinephrine and norepinephrine increase heart rate, breathing rate, cardiac muscle contractions, blood pressure, and blood glucose levels. They also accelerate the breakdown of glucose in skeletal muscles and stored fats in adipose tissue.
The release of epinephrine and norepinephrine is stimulated by neural impulses from the sympathetic nervous system. Secretion of these hormones is stimulated by acetylcholine release from preganglionic sympathetic fibers innervating the adrenal medulla. These neural impulses originate from the hypothalamus in response to stress to prepare the body for the fight-or-flight response.
Other notable endocrine glands
Some other notable endocrine glands include the parathyroid gland, pancreas, pineal glands, and gonads. You will find brief summaries of each of these glands, respectively, below.
Let’s start with the parathyroid gland, which most people have two to six of. The parathyroid gland, fittingly, secretes a hormone called parathyroid hormone which is responsible for increasing blood calcium levels. Parathyroid hormone (1) enhances reabsorption of Ca2+ by the kidneys, (2) stimulates osteoclast activity and inhibits osteoblast activity, and (3) it stimulates synthesis and secretion of calcitriol by the kidneys, which enhances Ca2+ absorption by the digestive system.
Next we also have the pancreas which secretes two key hormones responsible for regulating blood glucose levels. The pancreatic islets contain two primary cell types: alpha cells, which produce the hormone glucagon, and beta cells, which produce the hormone insulin. These hormones regulate blood glucose levels. As blood glucose levels decline, alpha cells release glucagon to raise the blood glucose levels by increasing rates of glycogen breakdown and glucose release by the liver. When blood glucose levels rise, such as after a meal, beta cells release insulin to lower blood glucose levels by increasing the rate of glucose uptake in most body cells, and by increasing glycogen synthesis in skeletal muscles and the liver. Together, glucagon and insulin regulate blood glucose levels.
Thirdly, we have the pineal gland which secretes melatonin (Note that melatonin and serotonin are both derived from an essential amino acid called tryptophan). In some mammals, melatonin has an inhibitory affect on reproductive functions by decreasing production and maturation of sperm, oocytes, and reproductive organs. Melatonin is an effective antioxidant, protecting the CNS from free radicals such as nitric oxide and hydrogen peroxide. Lastly, melatonin is involved in biological rhythms, particularly circadian rhythms such as the sleep-wake cycle and eating habits.
Lastly, we will briefly discuss the gonads. The gonads—the testes and ovaries in males and females, respectively—produce steroid hormones. The testes produce androgens, testosterone being the most prominent, which allow for the growth and development of the testes and penis, increased skeletal and muscular growth, enlargement of the larynx, increased growth and redistribution of body hair, and the production of sperm cells. The ovaries produce some testosterone, estradiol and progesterone, which cause secondary sex characteristics and prepare the body for childbirth.
Reading Question #5
An individual with Diabetes Type I cannot produce ________ and therefore, may experience high blood glucose levels. Which hormone is not produced in individuals with Type I diabetes?
A. Insulin
B. Glucagon
C. Parathyroid hormone
D. Thyroid hormone
Plant Responses to Light
Plants have a number of sophisticated uses for light that go far beyond their ability to photosynthesize low-molecular-weight sugars using only carbon dioxide, light, and water. Phototropism is a directional response that allows plants to grow towards, or even away from, light. Positive phototropism is growth towards a light source (Figure 20.3), while negative phototropism (also called skototropism) is growth away from light. The sensing of light in the environment is important to plants; it can be crucial for competition and survival. The response of plants to light is mediated by different photoreceptors.

Plant Responses to Gravity
Whether or not they germinate in the light or in total darkness, shoots usually sprout up from the ground, and roots grow downward into the ground. A plant laid on its side in the dark will send shoots upward when given enough time. Gravitropism ensures that roots grow into the soil and that shoots grow toward sunlight. Growth of the shoot apical tip upward is called negative gravitropism, whereas growth of the roots downward is called positive gravitropism.
Amyloplasts (also known as statoliths) are specialized plastids that contain starch granules and settle downward in response to gravity. Amyloplasts are found in shoots and in specialized cells of the root cap. When a plant is tilted, the statoliths drop to the new bottom cell wall. A few hours later, the shoot or root will show growth in the new vertical direction.
The mechanism that mediates gravitropism is reasonably well understood. When amyloplasts settle to the bottom of the gravity-sensing cells in the root or shoot, they physically contact the endoplasmic reticulum (ER), causing the release of calcium ions from inside the ER. This calcium signaling in the cells causes polar transport of the plant hormone IAA to the bottom of the cell. In roots, a high concentration of IAA inhibits cell elongation. The effect slows growth on the lower side of the root, while cells develop normally on the upper side. IAA has the opposite effect in shoots, where a higher concentration at the lower side of the shoot stimulates cell expansion, causing the shoot to grow up. After the shoot or root begin to grow vertically, the amyloplasts return to their normal position. Other hypotheses—involving the entire cell in the gravitropism effect—have been proposed to explain why some mutants that lack amyloplasts may still exhibit a weak gravitropic response.
Auxins
The term auxin is derived from the Greek word auxein, which means “to grow.” Auxins are the main hormones responsible for cell elongation in phototropism and gravitropism. They also control the differentiation of meristem into vascular tissue, and promote leaf development and arrangement. While many synthetic auxins are used as herbicides, IAA is the only naturally occurring auxin that shows physiological activity. Apical dominance—the inhibition of lateral bud formation—is triggered by auxins produced in the apical meristem. Flowering, fruit setting and ripening, and inhibition of abscission (leaf falling) are other plant responses under the direct or indirect control of auxins.
Commercial use of auxins is widespread in plant nurseries and for crop production. IAA is used as a rooting hormone to promote growth of adventitious roots on cuttings and detached leaves. Applying synthetic auxins to tomato plants in greenhouses promotes normal fruit development. Outdoor application of auxin promotes synchronization of fruit setting and dropping to coordinate the harvesting season. Fruits such as seedless cucumbers can be induced to set fruit by treating unfertilized plant flowers with auxins.
Plant Responses to Wind and Touch
The shoot of a pea plant winds around a trellis, while a tree grows on an angle in response to strong prevailing winds. These are examples of how plants respond to touch or wind.
The movement of a plant subjected to constant directional pressure is called thigmotropism, from the Greek words thigma meaning “touch,” and tropism implying “direction.” Tendrils are one example of this. The meristematic region of tendrils is very touch sensitive; light touch will evoke a quick coiling response. Cells in contact with a support surface contract, whereas cells on the opposite side of the support expand. Application of jasmonic acid is sufficient to trigger tendril coiling without a mechanical stimulus.
A thigmonastic response is a touch response independent of the direction of stimulus. In the Venus flytrap, two modified leaves are joined at a hinge and lined with thin fork-like tines along the outer edges. Tiny hairs are located inside the trap. When an insect brushes against these trigger hairs, touching two or more of them in succession, the leaves close quickly, trapping the prey. Glands on the leaf surface secrete enzymes that slowly digest the insect. The released nutrients are absorbed by the leaves, which reopen for the next meal.
Thigmomorphogenesis is a slow developmental change in the shape of a plant subjected to continuous mechanical stress. When trees bend in the wind, for example, growth is usually stunted and the trunk thickens. Strengthening tissue, especially xylem, is produced to add stiffness to resist the wind’s force. Researchers hypothesize that mechanical strain induces growth and differentiation to strengthen the tissues. Ethylene and jasmonate are likely involved in thigmomorphogenesis.
References
Adapted from Clark, M.A., Douglas, M., and Choi, J. (2018). Biology 2e. OpenStax. Retrieved from https://openstax.org/books/biology-2e/pages/1-2-themes-and-concepts-of-biology?query=%22organ%20system%22&target=%7B%22type%22%3A%22search%22%2C%22index%22%3A0%7D#fs-id2155753
Barrickman, N., Bell, K., and Cowan, C. (n.d.) Human Biology. Pressbooks. Retrieved from https://slcc.pressbooks.pub/humanbiology/chapter/chapter-12-organ-systems-of-the-human-body/
Lumen Learning. (2021). Fundamentals of Biology I. https://library.achievingthedream.org/herkimerbiologyfundamentals1/chapter/plant-sensory-systems-and-responses/
5.1: Organs and systems of the human organism. (2019, February 18). Medicine LibreTexts; Libretexts. https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Book%3A_Human_Anatomy_and_Physiology_Preparatory_Course_(Liachovitzky)/05%3A_Higher_Levels_of_Complexity-_Organs_and_Systems/5.01%3A_Organs_and_Systems_of_the_Human_Organism
Adapted from Clark, M.A., Douglas, M., and Choi, J. (2018). Biology 2e. OpenStax. Retrieved from https://openstax.org/books/biology-2e/pages/1-introduction

