30 Chapter 30: Gametogenesis and Sexual Reproduction
Anastasia Chouvalova and Mason Tedeschi
Learning Objectives
By the end of this chapter, you should be able to
Gametogenesis
Gametogenesis, the production of sperm and eggs, takes place through the process of meiosis. During meiosis, two cell divisions separate the paired chromosomes in the nucleus and then separate the chromatids that were made during an earlier stage of the cell’s life cycle. Meiosis produces haploid cells with half of each pair of chromosomes normally found in diploid cells. The production of sperm is called spermatogenesis and the production of eggs is called oogenesis.
Spermatogenesis
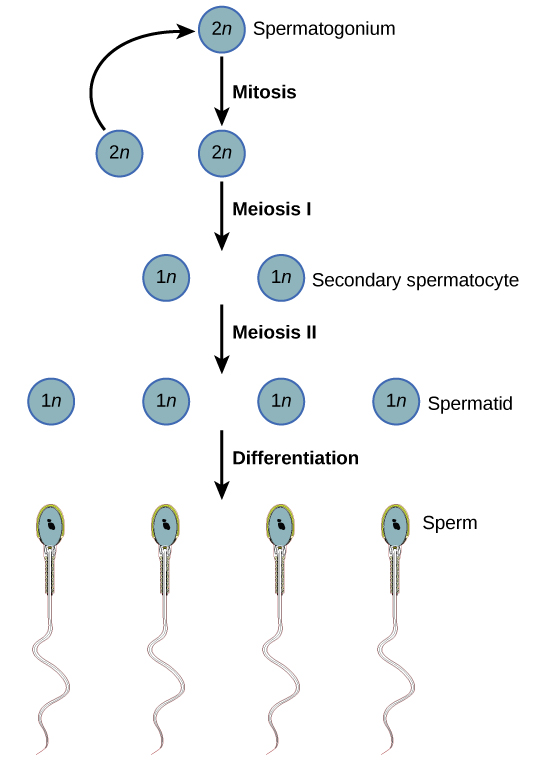
Meiosis starts with a cell called a primary spermatocyte. At the end of the first meiotic division, a haploid cell is produced called a secondary spermatocyte. This cell is haploid and must go through another meiotic cell division. The cell produced at the end of meiosis is called a spermatid and when it reaches the lumen of the tubule and grows a flagellum, it is called a sperm cell. Four sperm result from each primary spermatocyte that goes through meiosis.
Stem cells are deposited during gestation and are present at birth through the beginning of adolescence, but in an inactive state. During adolescence, gonadotropic hormones from the anterior pituitary cause the activation of these cells and the production of viable sperm. This continues into old age.
Link to Learning
Visit this site to see the process of spermatogenesis in more detail.
Oogenesis
Oogenesis, illustrated in Figure 30.2, occurs in the outermost layers of the ovaries. As with sperm production, oogenesis starts with a germ cell, called an oogonium (plural: oogonia), but this cell undergoes mitosis to increase in number, eventually resulting in up to about one to two million cells in the embryo.
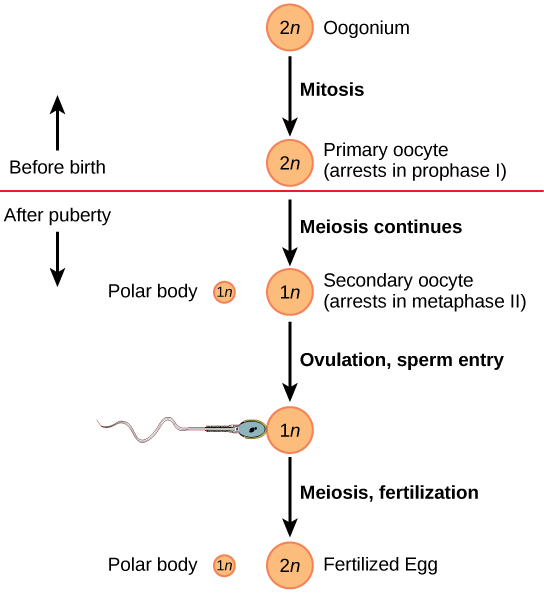
The cell starting meiosis is called a primary oocyte, as shown in Figure 30.2. This cell will start the first meiotic division and be arrested in its progress in the first prophase stage. At the time of birth, all future eggs are in the prophase stage. At adolescence, anterior pituitary hormones cause the development of a number of follicles in an ovary. This results in the primary oocyte finishing the first meiotic division. The cell divides unequally, with most of the cellular material and organelles going to one cell, called a secondary oocyte, and only one set of chromosomes and a small amount of cytoplasm going to the other cell. This second cell is called a polar body and usually dies. A secondary meiotic arrest occurs, this time at the metaphase II stage. At ovulation, this secondary oocyte will be released and travel toward the uterus through the oviduct. If the secondary oocyte is fertilized, the cell continues through the meiosis II, producing a second polar body and a fertilized egg containing all 46 chromosomes of a human being, half of them coming from the sperm.
Egg production begins before birth, is arrested during meiosis until puberty, and then individual cells continue through at each menstrual cycle. One egg is produced from each meiotic process, with the extra chromosomes and chromatids going into polar bodies that degenerate and are reabsorbed by the body.
Reading Question #1
Which of the following statements accurately describes a key difference between oogenesis and spermatogenesis?
A. Spermatogenesis produces polar bodies while oogenesis does not produce polar bodies.
B. In oogenesis, each meiosis round produces only one egg while in spermatogenesis, each meiosis round produces four sperm.
C. In oogenesis, each meiosis round produces four egg while in spermatogenesis, each meiosis round produces one sperm.
D. Spermatogenesis yields haploid cells while oogenesis yields diploid cells.
Sexual Reproduction in Animals
Animal reproduction is necessary for the survival of a species. In the animal kingdom, there are innumerable ways that species reproduce. Asexual reproduction produces genetically identical organisms (clones), whereas in sexual reproduction, the genetic material of two individuals combines to produce offspring that are genetically different from their parents.
Generally, the producers of sperm (the small gamete) are called males, producers of the eggs (the large gamete) are called females. Any other characteristics that may often be associated with sex, such as parental care or sexual behavior, are not universal throughout the animal kingdom. During sexual reproduction the male gamete (sperm) may be placed inside the female’s body for internal fertilization, or the sperm and eggs may be released into the environment for external fertilization. Seahorses provide an example of the latter. Following a mating dance, the female lays eggs in the male seahorse’s abdominal brood pouch where they are fertilized. The eggs hatch and the offspring develop in the pouch for several weeks.
Hormonal Regulation of the Reproductive System
Regulation of the reproductive system is a process that requires the action of hormones from the pituitary gland, the adrenal cortex, and the gonads. During puberty in both males and females, the hypothalamus produces gonadotropin-releasing hormone (GnRH), which stimulates the production and release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. These hormones regulate the gonads (testes in males and ovaries in females) and therefore are called gonadotropins. In both males and females, FSH stimulates gamete production and LH stimulates production of hormones by the gonads. An increase in gonad hormone levels inhibits GnRH production through a negative feedback loop.
Regulation of the Testicular Reproductive System
In the testes, FSH stimulates the maturation of sperm cells. FSH production is inhibited by the hormone inhibin, which is released by the testes. LH stimulates production of the sex hormones (androgens) by the interstitial cells of the testes and therefore is also called interstitial cell-stimulating hormone.
The most widely known androgen in males is testosterone. Testosterone promotes the production of sperm and a suite of secondary sex characteristics, such as the growth and development of the testes and penis, increased skeletal and muscular growth, enlargement of the larynx, increased growth and redistribution of body hair, and increased sexual drive. The adrenal cortex also produces small amounts of testosterone precursor, although the role of this additional hormone production is not fully understood. Testosterone secretion is regulated by both the hypothalamus and the anterior pituitary gland. The hypothalamus sends releasing hormones that stimulate the release of gonadotropins from the anterior pituitary gland.
Everyday Connection
The Dangers of Synthetic Hormones
Some athletes attempt to boost their performance by using artificial hormones that enhance muscle performance. Anabolic steroids, a form of testosterone, are one of the most widely known performance-enhancing drugs. Steroids are used in sports to help build muscle mass. Other hormones that are used to enhance athletic performance include erythropoietin, which triggers the production of red blood cells, and human growth hormone, which can help in building muscle mass. Most performance enhancing drugs are illegal for nonmedical purposes. They are also banned by national and international governing bodies including the International Olympic Committee, the U.S. Olympic Committee, the National Collegiate Athletic Association, the Major League Baseball, and the National Football League.
The side effects of synthetic hormones are often significant and nonreversible, and in some cases, fatal. Androgens can produce several complications such as liver dysfunctions and liver tumors, prostate gland enlargement, difficulty urinating, premature closure of epiphyseal cartilages, testicular atrophy, infertility, and immune system depression. The physiological strain caused by these substances is often greater than what the body can handle, leading to unpredictable and dangerous effects and linking their use to heart attacks, strokes, and impaired cardiac function.

Regulation of the Ovarian Reproductive System
In the ovaries, FSH stimulates development of egg cells, called ova, which develop in structures called follicles. Follicle cells produce the hormone inhibin, which inhibits FSH production. LH also plays a role in the development of ova, induction of ovulation, and stimulation of estradiol and progesterone production by the ovaries (as well as testosterone production by the testes), as illustrated in Figure 26.8. Estradiol and progesterone are steroid hormones that serve several functions in the human body. Estradiol causes the egg to mature and release during the menstrual cycle, and thickens the uterine lining prior to egg implantation. Estradiol also helps with bone health, nitric oxide production, and brain function. (Low levels of estradiol have been connected to osteoporosis, mood swings, weight gain, and interrupted menstrual cycle. High levels of estradiol correlate with an increased risk of uterine and breast cancer, and cardiovascular disease.) During puberty, estradiol produces a suite of characteristics such as the increased development of breast tissue, redistribution of fat towards hips, legs, and breast, and the maturation of the uterus and vagina. Both estradiol and progesterone regulate the menstrual cycle.
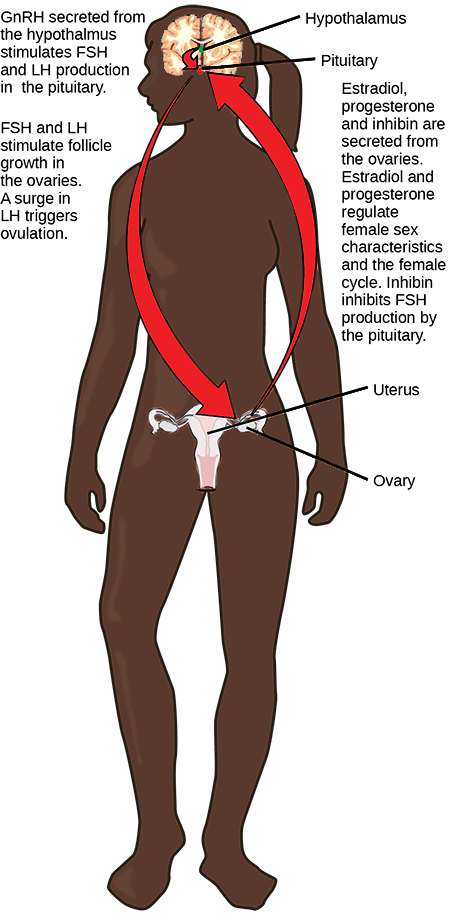
In addition to producing FSH and LH, the anterior portion of the pituitary gland also produces the hormone prolactin (PRL). Prolactin stimulates the production of milk by the mammary glands following childbirth. Prolactin release inhibits the release of GnRH from the hypothalamus, resulting in a loss of FSH and LH release from the anterior pituitary. Prolactin levels are regulated by the hypothalamic hormones prolactin-releasing hormone (PRH) and prolactin-inhibiting hormone (PIH), which is now known to be dopamine. PRH stimulates the release of prolactin and PIH inhibits it.
The posterior pituitary releases the hormone oxytocin, which stimulates uterine contractions during childbirth. (Note: the posterior pituitary secretes only two hormones: antidiuretic hormone (ADH and oxytocin). The uterine smooth muscles are not very sensitive to oxytocin until late in pregnancy when the number of oxytocin receptors in the uterus peaks. Stretching of tissues in the uterus and cervix stimulates oxytocin release during childbirth. Contractions increase in intensity as blood levels of oxytocin rise via a positive feedback mechanism until the birth is complete. Oxytocin also stimulates the contraction of myoepithelial cells around the milk-producing mammary glands. As these cells contract, milk is forced from the secretory alveoli into milk ducts and is ejected from the breasts in milk ejection (“let-down”) reflex. Oxytocin release is stimulated by the suckling of an infant, which triggers the synthesis of oxytocin in the hypothalamus and its release into circulation at the posterior pituitary.
Nearly all eukaryotes undergo sexual reproduction. The variation introduced into the reproductive cells by meiosis provides an important advantage that has made sexual reproduction evolutionarily successful. Meiosis and fertilization alternate in sexual life cycles. The process of meiosis produces unique reproductive cells called gametes, which have half the number of chromosomes as the parent cell. When two haploid gametes fuse, this restores the diploid condition in the new zygote. Thus, most sexually reproducing organisms alternate between haploid and diploid stages. However, the ways in which reproductive cells are produced and the timing between meiosis and fertilization vary greatly.
Reading Question #2
Match the function of the following hormones correctly.
A) Prolactin. B) Oxytocin. C) FSH. D) LH
- Important during childbirth due to the stimulation of uterine contraction and also in breastfeeding.
- Important in ovulation and stimulating ovarian hormone production.
- Important after childbirth due to the stimulation of milk production
- Important in stimulating egg cell development.
Menstruation
What Is the Menstrual Cycle?
The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years. The cycle is necessary for the production of eggs and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and the uterus and is controlled by pituitary and ovarian hormones. Day 1 of the cycle is the first day of the menstrual period, when bleeding from the uterus begins as the built-up endometrium lining the uterus is shed. The endometrium builds up again during the remainder of the cycle, only to be shed again during the beginning of the next cycle if pregnancy does not occur. In the ovaries, the menstrual cycle includes the development of a follicle, ovulation of a secondary oocyte, and the degeneration of the
Menarche and Menopause
The female reproductive years are delineated by the start and stop of the menstrual cycle. The first menstrual period usually occurs around 12 or 13 years of age, an event that is known as menarche. There is considerable variation among individuals in the age of menarche. It may occasionally occur as early as eight years of age or as late as 16 years of age and still be considered normal. The average age is generally later in the developing world, and earlier in the developed world. This variation is thought to be largely attributable to nutritional differences.
The cessation of menstrual cycles at the end of a woman’s reproductive years is termed menopause. The average age of menopause is 52 years, but it may occur normally at any age between about 45 and 55 years of age. The age of menopause varies due to a variety of biological and environmental factors. It may occur earlier as a result of certain illnesses or medical treatments.
Variation in the Menstrual Cycle
The length of the menstrual cycle— as well as its phases — may vary considerably, not only among different individuals but also from month to month for a given person. The average length of time between the first day of one menstrual period and the first day of the next menstrual period is 28 days, but it may range from 21 days to 45 days. Cycles are considered regular when a woman’s longest and shortest cycles differ by less than eight days. The menstrual period itself is usually about five days long, but it may vary in length from about two days to seven days.
Ovarian Cycle
The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It consists of changes that occur in the follicles of one of the ovaries. The ovarian cycle is divided into the following three phases: the follicular phase, ovulation, and luteal phase. These phases are illustrated in Figure 30.5.
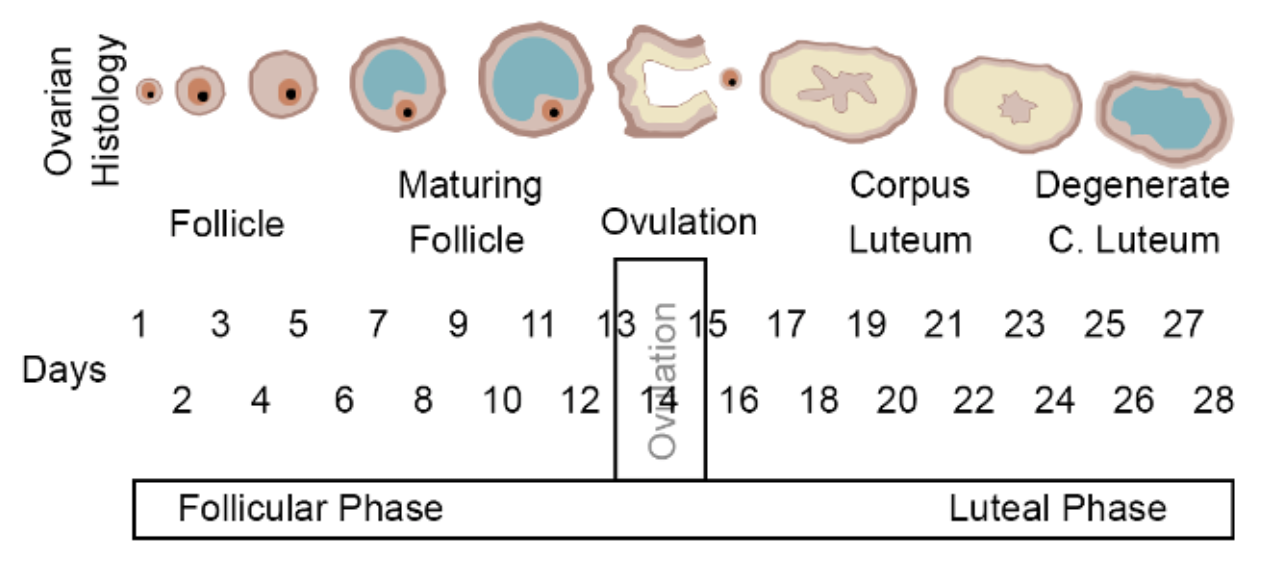
Follicular Phase
The follicular phase is the first phase of the ovarian cycle. It generally lasts about 12 to 14 days for a 28-day menstrual cycle. During this phase, several ovarian follicles are stimulated to begin maturing, but usually only one — called the Graafian follicle— matures completely so it is ready to release an egg. The other maturing follicles stop growing and disintegrate. Follicular development occurs because of a rise in the blood level of follicle-stimulating hormone (FSH), which is secreted by the pituitary gland. The maturing follicle releases estrogen, the level of which rises throughout the follicular phase. You can see these and other changes in hormone levels that occur during the menstrual cycle in the chart in Figure 30.6.
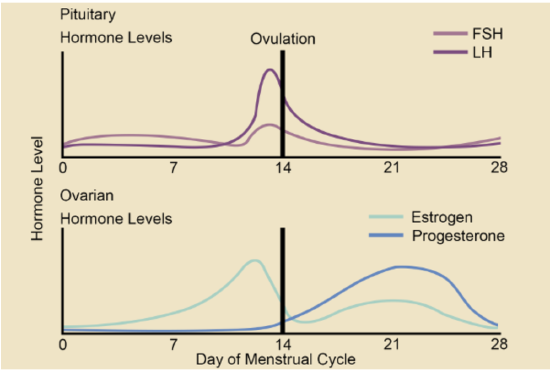
in the ovaries increase during the first half of themenstrual cycle. LH in the pituitary surges shortly before ovulation occurs due to the rise in estrogen in the ovaries. After ovulation, the level of progesterone and estrogen increases in ovaries due to the formation of the corpus luteum if pregnancy does not occur.
Ovulation
Luteal Phase
The luteal phase is the third and final phase of the ovarian cycle. It typically lasts about 14 days in a 28-day menstrual cycle. At the beginning of the luteal phase, FSH and LH cause the Graafian follicle that ovulated the egg to transform into a structure called a corpus luteum. The corpus luteum secretes progesterone, which in turn suppresses FSH and LH production by the pituitary and stimulates the continued buildup of the endometrium in the uterus. How this phase ends depends on whether or not the egg has been fertilized.
- If fertilization has not occurred, the falling levels of FSH and LH during the luteal phase cause the corpus luteum to atrophy, so its production of progesterone declines. Without a high level of progesterone to maintain it, the endometrium starts to break down. By the end of the luteal phase, the
endometrium can no longer be maintained, and the next menstrual cycle begins with the shedding of the endometrium (menses).
- If fertilization has occurred so a zygote forms and then divides to become a blastocyst, the outer layer of the blastocyst produces a hormone called human chorionic gonadotropin. This hormone is very similar to LH and preserves the corpus luteum. The corpus luteum can then continue to secrete progesterone to maintain the new pregnancy.
Uterine Cycle
The events of the menstrual cycle that take place in the uterus make up the uterine cycle. This cycle consists of changes that occur mainly in the endometrium, which is the layer of tissue that lines the uterus. The uterine cycle is divided into the following three phases: menstruation, proliferative phase, and secretory phase. These phases are illustrated in Figure 30.7.
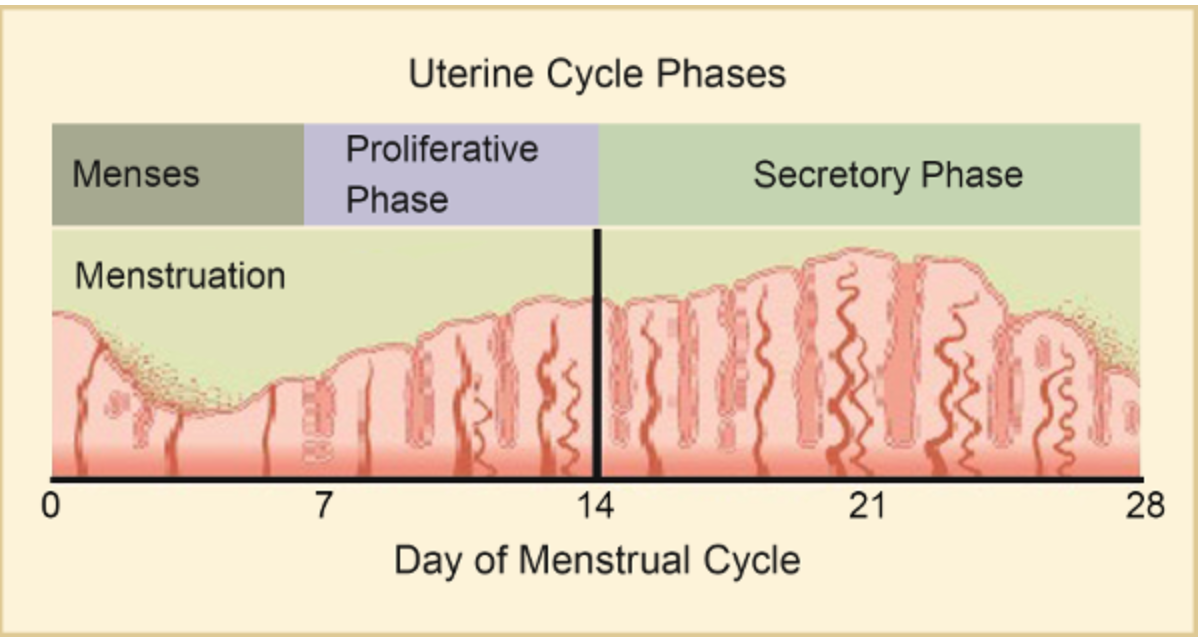
Menstruation
Proliferative Phase
The proliferative phase is the second phase of the uterine cycle. During this phase, estrogen secreted by cells of the maturing ovarian follicle
causes the lining of the uterus to grow, or proliferate. Estrogen also stimulates the cervix of the uterus to secrete larger amounts of thinner mucus that can help
Secretory Phase
The secretory phase is the third and final phase of the uterine cycle. During this phase, progesterone produced by the corpus luteum in the
Link to Society
Within the field of critical menstruation studies, we must pay attention to our depictions of menstruation and menstruators, and the knowledge we produce in the pursuit to de-stigmatize menstruation. Not all women menstruate, for example, trans women, postmenopausal women, pregnant women, and those experiencing amenorrhea, and not all who menstruate are women, for example, transmen. Experiences of menstruating later in life vary among menstruators as well. Some do not suffer from their periods in direct relation to their gender identity. Others do, as they disidentify with the body as a whole and/or with certain body parts such as the genitalia or the uterus, or with the bodily function of menstruation. This suffering is sometimes related to gender dysphoria. Testosterone treatments are a method adopted by some trans menstruators to get rid of unwanted bleeding. Preventing the menstrual period is not necessarily the main reason for using testosterone, but it can be one among several desired outcomes. Menstruators are of a variety of gender identities (far beyond those who identify as trans) and, hence, menstruation cannot be equated singularly with cis/womanhood.
Sexual reproduction in plants
Sexual reproduction takes place with slight variations in different groups of plants. Plants have two distinct stages in their lifecycle: the gametophyte stage and the sporophyte stage. The haploid gametophyte produces the male and female gametes by mitosis in distinct multicellular structures. Fusion of the male and females gametes forms the diploid zygote, which develops into the sporophyte. After reaching maturity, the diploid sporophyte produces spores by meiosis, which in turn divide by mitosis to produce the haploid gametophyte. The new gametophyte produces gametes, and the cycle continues. This is the alternation of generations, and is typical of plant reproduction (Figure 30.8).
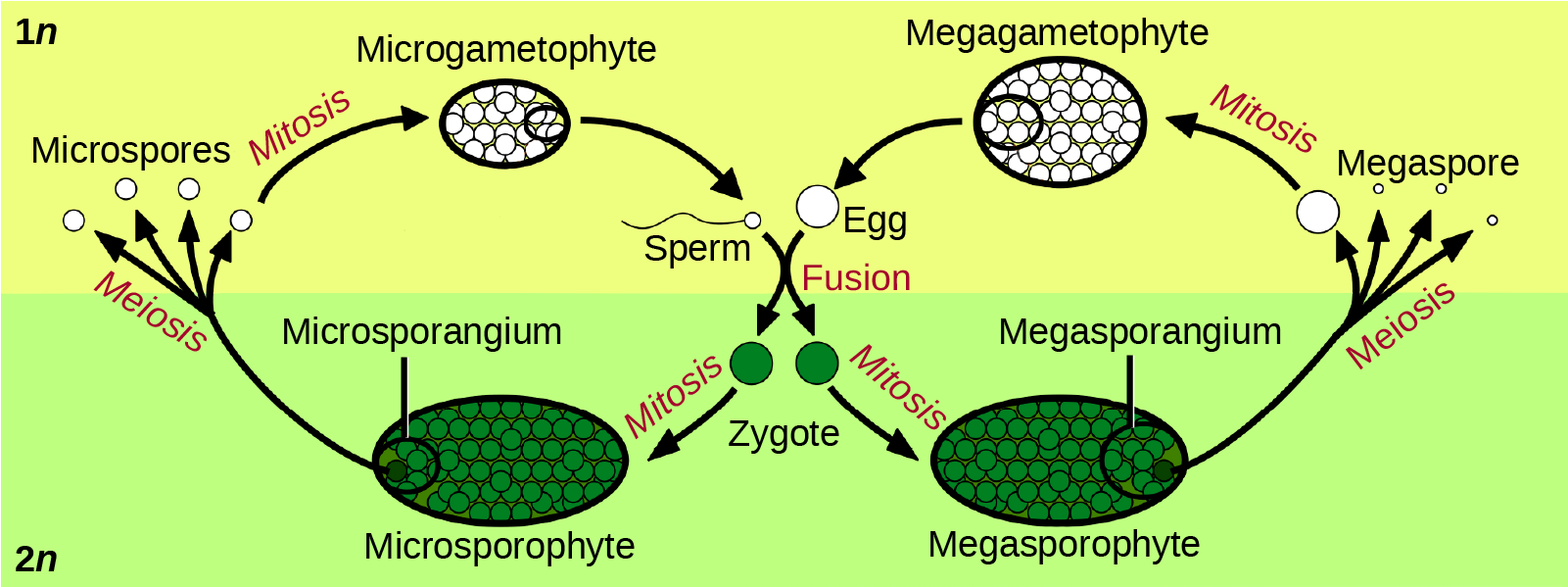
The life cycle of higher plants is dominated by the sporophyte stage, with the gametophyte borne on the sporophyte. In ferns, the gametophyte is free-living and very distinct in structure from the diploid sporophyte. In bryophytes, such as mosses, the haploid gametophyte is more developed than the sporophyte.
During the vegetative phase of growth, plants increase in size and produce a shoot system and a root system. As they enter the reproductive phase, some of the branches start to bear flowers. Many flowers are borne singly, whereas some are borne in clusters. The flower is borne on a stalk known as a receptacle. Flower shape, color, and size are unique to each species, and are often used by taxonomists to classify plants.
Sexual Reproduction in Angiosperms
The lifecycle of angiosperms follows the alternation of generations explained previously. The haploid gametophyte alternates with the diploid sporophyte during the sexual reproduction process of angiosperms. Flowers contain the plant’s reproductive structures.
Flower Structure
A typical flower has four main parts—or whorls—known as the calyx, corolla, androecium, and gynoecium (Figure 30.9). The outermost whorl of the flower has green, leafy structures known as sepals. The sepals, collectively called the calyx, help to protect the unopened bud. The second whorl is comprised of petals—usually, brightly colored—collectively called the corolla. The number of sepals and petals varies depending on whether the plant is a monocot or dicot. In monocots, petals usually number three or multiples of three; in dicots, the number of petals is four or five, or multiples of four and five. Together, the calyx and corolla are known as the perianth. The third whorl contains the male reproductive structures and is known as the androecium. The androecium has stamens with anthers that contain the microsporangia. The innermost group of structures in the flower is the gynoecium, or the female reproductive component(s). The carpel is the individual unit of the gynoecium and has a stigma, style, and ovary. A flower may have one or multiple carpels.
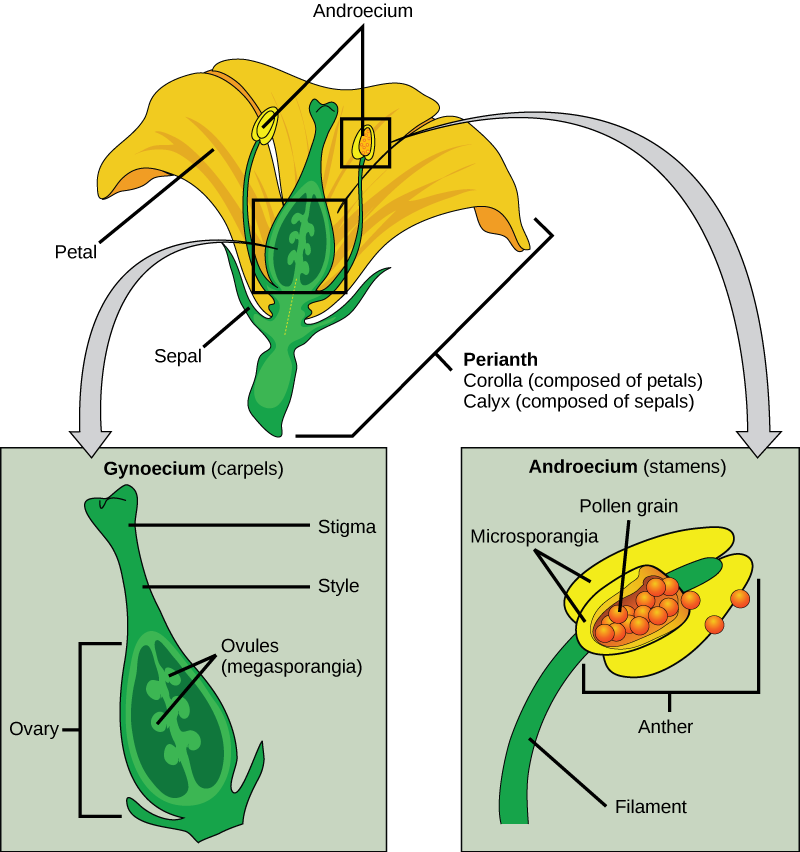
If all four whorls (the calyx, corolla, androecium, and gynoecium) are present, the flower is described as complete. If any of the four parts is missing, the flower is known as incomplete. Flowers that contain both an androecium and a gynoecium are called perfect, androgynous or hermaphrodites. There are two types of incomplete flowers: staminate flowers contain only an androecium, and carpellate flowers have only a gynoecium (Figure 30.10).

Reading Question #3
Which of the following statements is false about floral reproduction?
A. The process of producing spores necessitates meiosis.
B. Flowers have four main parts called the androecium, gynoecium, calyx, and corolla.
C. Hermaphrodite flowers do not exist.
d. The process of producing gametes necessitates mitosis.
Reading Question #4
Which of the following body systems is not directly involved with spermatogenesis?
A. Circulatory
B. Endocrine
C. Respiratory
D. Reproductive
Reading Question #5
In what ways can testosterone affect spermatogenesis?
A. It can halt/stop it
B. It can increase it
C. It does not cause a change
References
Adapted from Clark, M.A., Douglas, M., and Choi, J. (2018). Biology 2e. OpenStax. Retrieved from https://openstax.org/books/biology-2e/pages/1-introduction
https://socialsci.libretexts.org/Courses/Sacramento_City_College/SCC%3A_SOC_300_-_Introduction_to_Sociology_(Block)/Text/8%3A_Gender_and_Gender_Inequality/8.2%3A_Understanding_Sex_and_Gender
https://bio.libretexts.org/Bookshelves/Human_Biology/Book%3A_Human_Biology_(Wakim_and_Grewal)/22%3A_Reproductive_System/22.07%3A_Menstrual_Cycle